Modern healthcare is built to treat problems quickly.
It is not built to understand people deeply.
This gap becomes most visible when someone lives with a complex, chronic, or poorly defined condition. Patients often leave appointments feeling unheard, rushed, or reduced to a diagnosis code. This is not usually because doctors do not care. It is because the system was never designed to give them time.
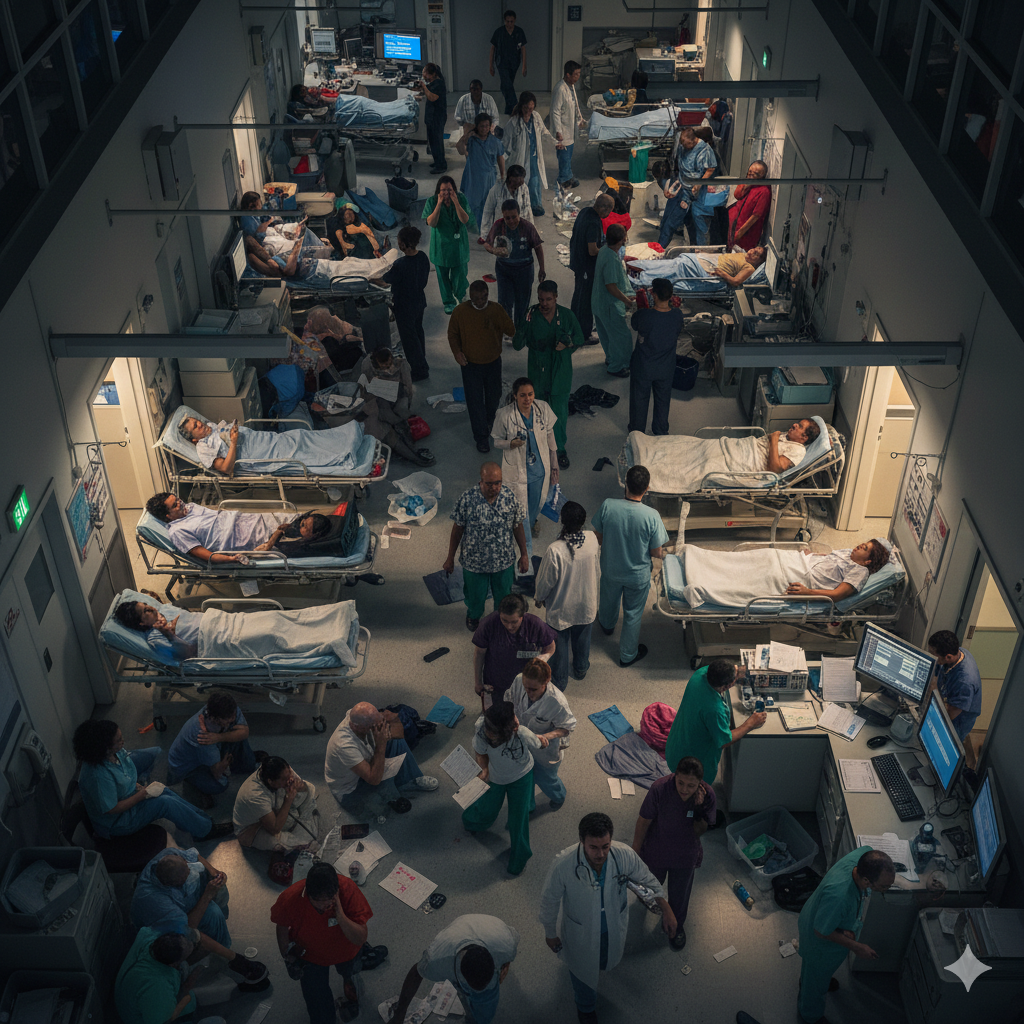
The Structural Time Problem in Modern Medicine
Most healthcare systems operate under strict time constraints:
- Appointments are commonly limited to 7–15 minutes
- Clinicians are expected to see high volumes of patients per day
- Performance is often measured by throughput, not understanding
- Administrative and documentation demands consume a large portion of clinicians’ time
In this context, depth becomes a luxury.
Understanding a person’s condition in a meaningful way often requires:
- listening to a long and non-linear story,
- exploring lifestyle, stress, sleep, work, and social context,
- acknowledging uncertainty and complexity,
- revisiting assumptions over time.
The system does not reward this. Speed is incentivized. Complexity is not.
Medicine Is Optimized for Acute Problems, Not Chronic Complexity
Modern healthcare developed extraordinary tools for:
- infections,
- trauma,
- emergencies,
- single-cause diseases with clear biomarkers.
Chronic conditions rarely follow this model.
Many long-term health issues involve:
- multiple interacting systems,
- fluctuating symptoms,
- unclear timelines,
- psychosocial and environmental factors,
- incomplete or conflicting scientific explanations.
These do not fit neatly into short consultations or standardized pathways. As a result, clinicians often have to simplify, narrow the focus, or rely on protocols that only capture part of the picture.
The Fragmentation of Care
Healthcare is highly specialized. Each professional sees a piece, not the whole:
- one appointment for pain,
- another for imaging,
- another for mental health,
- another for lifestyle advice.
No single encounter is designed to integrate everything into a coherent understanding of the person.
This fragmentation means that:
- context is lost between visits,
- stories are repeated but not always connected,
- responsibility for “the full picture” often falls on the patient.
The Knowledge Gap Is Not Personal — It’s Systemic
When patients feel misunderstood, it is easy to assume:
“My doctor doesn’t get it.”
More often, the reality is:
“The system doesn’t allow understanding to happen.”
Clinicians are trained within constraints:
- limited time,
- evolving and incomplete science,
- institutional protocols,
- legal and administrative pressures.
Even highly competent and compassionate professionals are working inside a structure that prioritizes efficiency over exploration.
Why This Matters for Patients
When understanding is shallow:
- symptoms may feel dismissed,
- explanations feel generic,
- uncertainty is uncomfortable for both sides,
- patients search elsewhere for meaning and answers.
This is one reason why people turn to:
- online communities,
- alternative frameworks,
- simplified narratives,
- or unverified explanations.
Not necessarily because they reject medicine, but because they seek understanding.
Education as a Missing Layer
Healthcare delivers treatments.
But understanding often requires education.
Education allows people to:
- see their condition within broader biological, psychological, and social systems,
- understand uncertainty without panic,
- distinguish between evidence, hypotheses, and speculation,
- engage with healthcare more critically and realistically.
This educational layer is rarely provided within clinical encounters — not due to lack of will, but lack of time.
A System Problem, Not a Moral One
This is not about blaming doctors.
It is about recognizing that modern healthcare was not designed to:
- sit with complexity,
- follow long narratives,
- or hold uncertainty over time.
Understanding chronic and complex conditions requires structures that medicine alone cannot currently provide.
Bridging that gap requires better education, better frameworks, and a clearer public understanding of what healthcare can — and cannot — realistically offer.
That is where platforms like HealthX360 focus their work:
not on replacing medical care, but on making complexity understandable.