Introduction
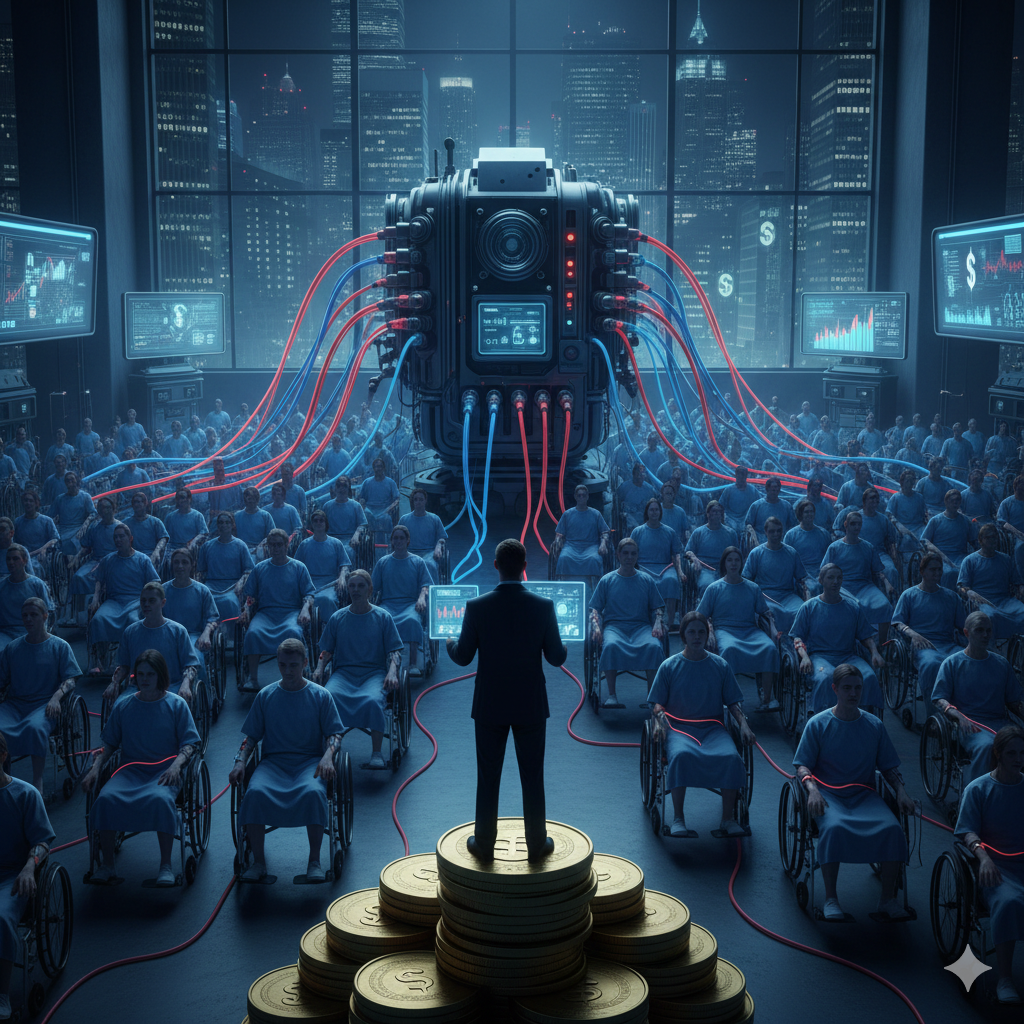
Modern healthcare is one of the largest industries in the world. In many countries, it represents 10–20% of national GDP, employing millions and generating trillions in annual revenue. Yet for patients living with chronic conditions, a disturbing pattern often emerges: symptoms are managed indefinitely, but root causes are rarely addressed.
This is not because clinicians are unethical or indifferent. It is because the healthcare system itself is structurally incentivized toward long-term dependency rather than long-term resolution.
Understanding these incentives is essential for anyone trying to make sense of why chronic patients often feel trapped in endless cycles of appointments, medications, and procedures.
Healthcare Is Designed as a Service Industry, Not a Recovery Industry
Healthcare systems—especially in high-income countries—operate primarily on volume-based models:
- More consultations = more revenue
- More prescriptions = more revenue
- More tests and procedures = more revenue
What is not directly rewarded is:
- Time spent understanding complex, multifactorial conditions
- Cross-disciplinary thinking
- Long-term functional recovery
- Patient education and health literacy
Chronic conditions, by definition, create recurring demand. From a systems perspective, a patient who requires lifelong management is economically more predictable than one who recovers and exits the system.
This is not a conspiracy. It is basic incentive design.
Chronic Illness Is Big Business
Globally, chronic diseases account for the majority of healthcare spending. Conditions such as chronic pain, diabetes, autoimmune disorders, cardiovascular disease, and mental health conditions generate continuous revenue streams through:
- Long-term medication use
- Repeat diagnostics and imaging
- Specialist referrals
- Follow-up appointments
- Interventional procedures
In this model:
- Acute problems are “solved.”
- Chronic problems are “managed.”
Management sustains the system. Resolution disrupts it.
Why Dependency Is Often Unintentional but Systemic
Most healthcare professionals enter medicine to help people. However, they work within constraints:
- 7–15 minute consultations
- Protocol-driven decision making
- Insurance and reimbursement limitations
- Fear of liability
- Fragmented specialties
These constraints reward speed, standardization, and symptom control, not complexity or uncertainty.
As a result:
- Patients become dependent on repeated external interventions
- Self-understanding and autonomy are rarely cultivated
- The system becomes the authority, not the patient’s own capacity to adapt, learn, and recover
Dependency emerges not from malice, but from structure.
The Pharmaceutical Feedback Loop
Medications are often life-saving and necessary. But in chronic care, they frequently become long-term substitutes for understanding.
Once a drug is prescribed:
- Side effects may require additional drugs
- Symptoms may shift rather than resolve
- Long-term use becomes normalized
Pharmaceutical business models depend on continuous use, not short-term cures. This creates a feedback loop where symptom suppression is favored over systemic inquiry.
Again, this is not about “evil corporations.” It is about business models aligning with dependency.
What’s Missing: Education, Context, and Systems Thinking
Most chronic conditions are multidimensional:
- Biological
- Psychological
- Social
- Environmental
- Behavioral
Yet care is usually delivered in isolated silos.
What patients rarely receive:
- Clear explanations of mechanisms
- Context for their symptoms
- Tools to interpret their own body signals
- Education that reduces fear and passivity
An informed patient is harder to keep dependent, but education is time-consuming and poorly reimbursed.
Why This Matters
When patients are not taught to understand their condition:
- They outsource authority entirely
- They lose confidence in their own body
- They become long-term consumers rather than active participants
Dependency is expensive—not just financially, but psychologically and socially.
A Different Direction: Health Literacy Over Dependency
Breaking dependency does not mean rejecting medicine. It means re-balancing the system toward:
- Education instead of endless intervention
- Understanding instead of blind compliance
- Long-term capacity instead of short-term relief
Healthcare should support patients until they need less of it, not indefinitely more.
Final Thought
The biggest problem in modern healthcare is not bad doctors or bad intentions.
It is misaligned incentives.
Until systems reward understanding, education, and long-term recovery, dependency will remain the default outcome—especially for chronic patients.
Recognizing this is the first step toward changing it.